Palliative Medicine holds vital relevance across every department and must be seamlessly integrated into the overall plan of care. Its scope is vast, inter-disciplinary and rooted in collaboration—uniting healthcare professionals to develop personalised care plans tailored to each patient’s unique needs and preferences.
Palliative care addresses the concept of ‘Total Pain’—a transformative, patient-centred approach that goes beyond physical symptoms to include emotional, psychosocial, and spiritual distress. It acknowledges not just the patient but also supports family members, caregivers, and loved ones, redefining the essence of healing with compassion.
Patients with complex, serious or life-limiting illnesses are more than their diagnoses—they are individuals with values, beliefs, experiences and challenges. This depth of need demands a holistic approach to care that complements conventional treatment, alleviates suffering, and enhances quality of life.
Contrary to popular belief, Palliative Care is not limited to End-of-Life care. It is a continuum of care that begins at the time of diagnosis and extends through Disease Directed Treatment, Terminal illness, End-of-Life Care, Death and into Bereavement Care for families. Early integration improves patient comfort, supports better decision-making, and enhances the effectiveness of other medical interventions.
Palliative Care Is a Right-for All Men and Women, Children and the elderly, Persons with disabilities, Hospitalised or chronically ill individuals.
Palliative Care has:
We offer robotic-assisted procedures across a wide range of specialities, including:

Pain is one of the most distressing symptoms in serious illnesses. Our team uses:
Our Pain Management and Palliative Care Department is dedicated to improving the quality of life for patients suffering from acute, chronic, cancer-related, or life-limiting pain. We combine interventional pain techniques with holistic palliative care to manage physical, emotional, and psychological distress-ensuring patient comfort at every stage of illness.









We provide individualised treatment plans for a wide range of pain-related conditions, including:
Back pain, fibromyalgia, sciatica, peripheral neuropathy, trigeminal neuralgia, phantom limb pain.
Osteoarthritis, rheumatoid arthritis, spondylolisthesis, myofascial pain syndrome, whiplash.
Migraines, cluster headaches, trigeminal neuralgia.
Cancer pain, mucositis, pancreatic cancer pain, radiation- or chemotherapy-induced pain.
Sickle cell disease-related pain, CRPS, vascular pain syndromes.
Degenerative disc disease, spinal stenosis, vertebral compression fractures, failed back surgery syndrome.
Osteomyelitis, shingles (herpes zoster), postoperative pain, hernia-related pain.
Chronic pancreatitis, endometriosis, interstitial cystitis, chronic pelvic pain syndrome.
Our Interventional Pain Centre offers advanced procedures performed by experienced specialists, including:
Epidural steroid injections, facet joint injections, sacroiliac joint blocks.
Medial branch blocks, sympathetic nerve blocks, nerve root blocks, radiofrequency ablation (RFA).
Vertebroplasty and kyphoplasty for spinal fractures, discography for discogenic pain evaluation.
Targeting muscle knots and myofascial trigger points to relieve localised muscle pain.
Chemical neurolysis for long-term relief in select chronic pain conditions.
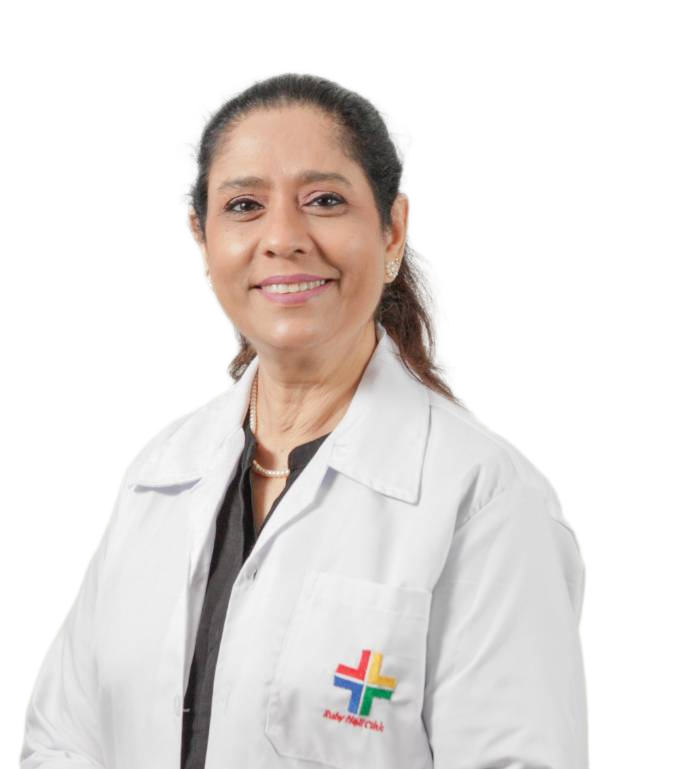
At our centre, we are proud to offer comprehensive care through a dedicated and experienced team of medical professionals. Our multidisciplinary team includes, but is not limited to:
– Clinical Psychologist
– Qualified Physiotherapists and Occupational Therapists
– Certified Dieticians
– Additional Specialists as required, based on individual patient needs
This collaborative approach ensures that each patient receives personalised, holistic and evidence-based care tailored to their specific condition.